Experiencing a thrombosed hemorrhoid can be intensely painful and concerning for many individuals. Unlike regular hemorrhoids, thrombosed hemorrhoids occur when a blood clot forms inside the hemorrhoid, leading to severe discomfort and distinctive symptoms that require prompt attention.
The most common signs of a thrombosed hemorrhoid include sudden, severe pain around the anus, a hard lump near the anal opening that may appear purple or blue, and significant swelling that makes sitting and daily activities extremely uncomfortable. These symptoms typically develop rapidly, often within 24-48 hours, distinguishing them from standard hemorrhoids.
For those experiencing these symptoms in New York City, LocalMD offers specialized care for hemorrhoid conditions. Their medical professionals can provide proper diagnosis and treatment options ranging from conservative management to surgical intervention when necessary.
What Is a Thrombosed Hemorrhoid?
A thrombosed hemorrhoid occurs when a blood clot forms inside a hemorrhoid, causing intense pain, swelling, and a bluish-purple color at the site. This painful condition typically develops rapidly and requires prompt attention to manage symptoms effectively.
Difference Between Regular and Thrombosed Hemorrhoids
Regular hemorrhoids are swollen veins in the lower rectum or around the anus that cause discomfort, itching, and occasional bleeding. They appear as soft, pliable tissue that may protrude during bowel movements.
Thrombosed hemorrhoids, however, contain a hard blood clot within the vein. This clot creates significant pressure, resulting in severe pain that regular hemorrhoids don’t typically cause. The appearance is distinctive—thrombosed hemorrhoids often look like a firm lump with a dark bluish color due to the trapped blood.
The pain from a thrombosed hemorrhoid typically peaks 48-72 hours after formation, then gradually subsides as the body reabsorbs the clot. Without treatment, this natural resolution process may take 2-3 weeks.
How Thrombosed Hemorrhoids Develop
Thrombosed hemorrhoids develop when blood flow within a hemorrhoidal vein becomes restricted, allowing blood to pool and clot. Several factors increase this risk, including prolonged sitting or standing, chronic constipation, and straining during bowel movements.
Pressure from pregnancy or obesity can significantly contribute to their formation. The straining forces blood into the hemorrhoidal vessels while simultaneously restricting outflow, creating ideal conditions for clot formation.
Activities that increase abdominal pressure, such as heavy lifting or intense physical exertion, may trigger the development of a thrombosed hemorrhoid. Once the clot forms at the base of the hemorrhoid, inflammation quickly follows, causing the characteristic severe pain and swelling.
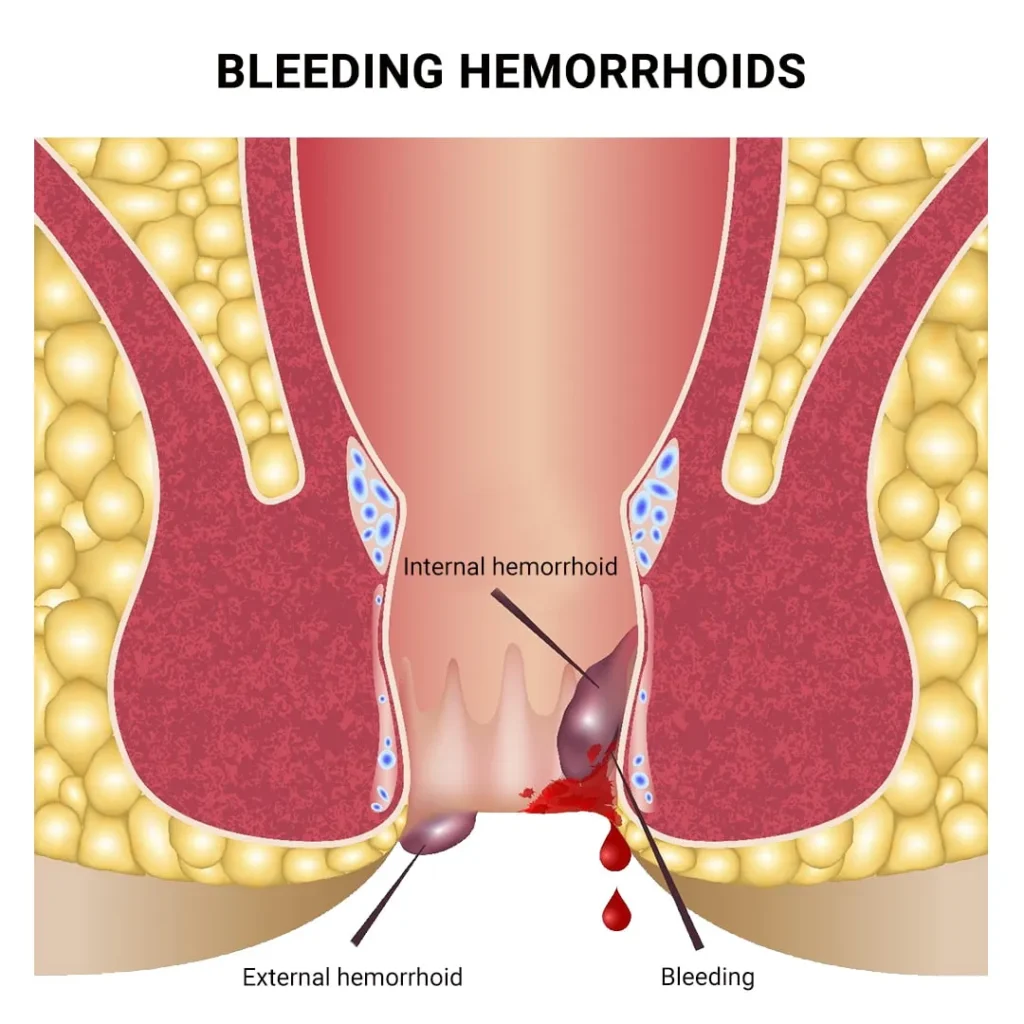
Types: Internal vs. External Thrombosed Hemorrhoids
External thrombosed hemorrhoids form around the anus, outside the anal canal, making them visible and particularly painful. These occur in veins covered by sensitive skin with abundant nerve endings, explaining the intense discomfort they cause.
The blood clot in external thrombosed hemorrhoids creates a hard, painful lump that’s tender to touch and may interfere with sitting or walking. They’re most common and easily identified due to their location and distinctive appearance.
Internal thrombosed hemorrhoids develop inside the anal canal above the dentate line. While less common, these can be equally problematic, causing pain, bleeding, and sometimes prolapse (protrusion through the anal opening). Because they form in an area with fewer pain receptors, they may initially cause less pain but can lead to complications if they prolapse or become severely inflamed.
Top Signs and Symptoms of a Thrombosed Hemorrhoid
Thrombosed hemorrhoids occur when blood clots form inside an external hemorrhoid, causing significant discomfort and distinctive physical symptoms. Recognizing these symptoms early allows for prompt treatment and relief.
Severe Anal Pain
The hallmark symptom of a thrombosed hemorrhoid is sudden, severe pain in the anal region. This pain is typically more intense than with regular hemorrhoids and can be described as sharp, throbbing, or constant.
The discomfort often begins abruptly and may worsen when sitting or during bowel movements. Many patients report that the pain is most severe within the first 48-72 hours after the blood clot forms.
Over-the-counter pain medications may provide minimal relief. The pain gradually subsides over approximately 7-10 days as the body naturally absorbs the clot, though complete resolution may take longer.
Swelling Around the Anus
Significant swelling accompanies thrombosed hemorrhoids, creating visible and palpable enlargement around the anus. This swelling often develops rapidly, sometimes within hours.
The affected area becomes tender to touch and may feel firm due to the blood clot. Patients typically notice increased sensitivity when cleaning the area or during physical activities.
This swelling can cause difficulty with sitting and may create a sensation of pressure or fullness in the rectal area. Unlike regular hemorrhoids, the swelling from thrombosed hemorrhoids tends to be more pronounced and localized.
Bluish or Purplish Lump
A distinctive feature of thrombosed hemorrhoids is the appearance of a bluish or purplish lump near the anal opening. This discoloration results from the blood clot trapped within the hemorrhoid.
The lump is typically firm to the touch and clearly visible upon examination. It may range in size from a pea to a marble, depending on the extent of the clotting.
This discolored lump differentiates thrombosed hemorrhoids from other anal conditions. As healing progresses, the color may change from dark purple to lighter shades before gradually resolving.
Rectal Bleeding
Though less common than with internal hemorrhoids, thrombosed hemorrhoids may cause minimal bleeding. When bleeding occurs, it typically appears as bright red blood on toilet paper or in the toilet bowl.
The bleeding results from pressure on the affected tissue or minor tears in the anal lining. Unlike internal hemorrhoid bleeding, which can be painless, bleeding from thrombosed hemorrhoids usually accompanies pain.
If the thrombosed hemorrhoid ruptures, more significant bleeding may occur, though this actually provides relief as pressure from the clot is released. Persistent or heavy bleeding should prompt immediate medical attention to rule out more serious conditions.
Causes and Risk Factors for Thrombosed Hemorrhoids
Thrombosed hemorrhoids develop when blood clots form inside hemorrhoidal veins, leading to intense pain and swelling. Several specific factors contribute to this condition, with pressure on anal veins being the primary underlying mechanism.
Increased Pressure on Anal Veins
The fundamental cause of thrombosed hemorrhoids is excessive pressure on the veins in the anal region. This pressure can result from various activities and conditions that strain the lower rectum. Heavy lifting, especially when performed incorrectly, significantly increases intra-abdominal pressure that transfers to the anal veins.
Pregnancy represents a major risk factor, particularly during the third trimester when the growing uterus puts substantial pressure on pelvic veins. This pressure can impede normal blood flow, causing veins to swell.
Obesity also contributes to increased pressure on anal veins, as excess weight creates constant strain on the lower body’s vascular system. Specialists at LocalMD NYC often identify weight management as a key preventive measure for recurrent hemorrhoid issues.
Chronic Constipation or Straining
Chronic constipation plays a significant role in the development of thrombosed hemorrhoids. When hard stool accumulates in the rectum, individuals tend to strain during bowel movements, creating intense pressure on anal veins.
This straining disrupts normal blood flow patterns in the anal cushions. Over time, repeated straining weakens the supporting tissues around hemorrhoidal veins, making them more susceptible to thrombosis.
Insufficient dietary fiber represents a major contributor to constipation-related hemorrhoids. Most adults need 25-30 grams of fiber daily, yet many consume less than half this amount.
Inadequate hydration further compounds constipation issues. Without proper fluid intake, stool becomes harder and more difficult to pass, requiring greater straining during bowel movements.
Prolonged Sitting or Sedentary Lifestyle
Sitting for extended periods significantly increases the risk of developing thrombosed hemorrhoids. Long periods of sitting place constant pressure on the anal region, restricting blood flow and promoting swelling of hemorrhoidal veins.
Occupations requiring prolonged sitting, such as office work or long-distance driving, create particular risk. The seated position compresses veins in the anal area, potentially leading to blood pooling and clot formation.
Lack of regular physical activity compounds these risks. Exercise promotes healthy circulation throughout the body, including the rectal area. Without this circulation benefit, blood can stagnate in hemorrhoidal veins.
Even short walking breaks during a sedentary day can significantly reduce risk. Movement stimulates blood flow and helps prevent the stasis that often precedes thrombosis in hemorrhoidal veins.
Treatment Options for Thrombosed Hemorrhoids
Managing thrombosed hemorrhoids involves a combination of at-home care and medical interventions. Treatment approaches range from simple self-care measures to more invasive procedures depending on the severity of symptoms.
At-Home Relief Methods
Sitz baths provide significant relief for many sufferers. Soaking the anal area in warm water for 10-15 minutes, 2-3 times daily, helps reduce inflammation and eases pain. This simple therapy increases blood flow to the area, promoting healing.
Cold therapy offers another approach. Applying ice packs wrapped in a cloth to the affected area for 15-20 minutes several times daily helps numb the area and reduce swelling.
Pain management typically involves over-the-counter medications like acetaminophen or ibuprofen. These help control discomfort while the thrombosed hemorrhoid heals naturally.
Dietary modifications play a crucial role in recovery. Increasing fiber intake through supplements or fiber-rich foods prevents constipation, reducing strain during bowel movements. Drinking plenty of water aids this process significantly.
Medical Procedures and Surgical Interventions
External thrombectomy represents a common medical procedure for thrombosed hemorrhoids. A doctor makes a small incision to remove the blood clot, providing immediate pain relief. This procedure works best when performed within 72 hours of symptom onset.
Hemorrhoidectomy becomes necessary for severe or recurring cases. This surgical procedure removes the hemorrhoid tissue completely and proves highly effective for long-term relief.
Rubber band ligation offers a less invasive option for internal hemorrhoids that have prolapsed. A doctor places a small rubber band around the hemorrhoid’s base, cutting off blood flow until it shrinks and falls off.
Many patients in Queens and Brooklyn find relief through specialized treatments at LocalMD clinics (Maspeth: 718-841-0874, Brooklyn: 718-550-8091), where doctors offer personalized care plans.
When to Seek Medical Attention
Severe pain that doesn’t improve with home treatments within 2-3 days warrants medical evaluation. Thrombosed hemorrhoids typically cause intense discomfort that should gradually diminish.
Bleeding from the rectum requires prompt medical assessment, even if mild. While some bleeding may occur with thrombosed hemorrhoids, anything persistent or heavy needs professional evaluation.
Fever or pus near the anal area indicates possible infection and demands immediate medical attention. These symptoms suggest complications beyond standard hemorrhoid issues.
Most thrombosed hemorrhoids resolve within 1-2 weeks with proper care. However, seeking timely medical advice prevents unnecessary suffering and reduces the risk of complications or recurrence.
Frequently Asked Questions
Patients with thrombosed hemorrhoids often have questions about their condition, symptoms, and treatment options. Below are answers to common questions that can help individuals better understand this painful condition.
What are the distinguishing features of a thrombosed hemorrhoid compared to regular hemorrhoids?
Thrombosed hemorrhoids appear as a hard, purple or blue lump at the anal opening due to clotted blood inside the hemorrhoid. They cause severe, constant pain unlike regular hemorrhoids which typically only hurt during bowel movements or when pressure is applied.
How long does it usually take for a thrombosed hemorrhoid to heal?
Without surgical intervention, thrombosed hemorrhoids typically resolve within 7-14 days as the body gradually absorbs the blood clot. Relief from severe pain usually occurs within 2-3 days, though complete healing may take longer.
What is the recommended treatment for thrombosed hemorrhoids?
Treatment options include conservative management with sitz baths, pain relievers, and stool softeners. External thrombosed hemorrhoids causing severe pain may benefit from surgical excision within 72 hours of symptom onset, which specialists at medical centers can perform.
Are there risks associated with thrombosed hemorrhoids that warrant immediate medical attention?
Immediate medical attention is necessary if there is excessive bleeding, severe uncontrolled pain, fever, inability to urinate, or significant swelling that prevents bowel movements. These symptoms may indicate complications requiring urgent intervention.
What conditions can be confused with thrombosed hemorrhoids upon examination?
Conditions often confused with thrombosed hemorrhoids include anal fissures, perianal abscesses, anal cancer, rectal prolapse, and anal warts. Proper diagnosis by a healthcare professional is essential to ensure appropriate treatment.
Can thrombosed hemorrhoids induce systemic symptoms or general malaise?
Thrombosed hemorrhoids typically do not cause systemic symptoms like fever or general malaise. If these symptoms occur alongside anal pain, it may indicate a different condition such as an infection or abscess requiring prompt medical evaluation.