Hernias affect millions of people worldwide, occurring when organs or tissues push through weakened areas in the surrounding muscle or connective tissue. While some hernias cause minimal discomfort and can be managed conservatively, others develop complications that make surgical intervention necessary.
A hernia occurs when part of an internal organ protrudes through a muscle opening or weakness, and surgical repair becomes necessary when the hernia causes significant symptoms, grows larger, or risks serious complications like incarceration or strangulation. The decision for surgical treatment depends on multiple factors including the type of hernia, severity of symptoms, and individual patient circumstances.
Understanding the different types of hernias, when surgery becomes essential, and what patients can expect from repair procedures helps individuals make informed decisions about their healthcare. Modern surgical techniques offer effective solutions with good outcomes, though prevention strategies and proper risk factor management remain important considerations for long-term hernia care.
Understanding Hernias and When Surgical Repair May Be Needed
Hernias develop when internal organs push through weakened muscle walls, creating visible bulges that often require surgical intervention. The decision for surgical repair depends on the hernia‘s location, size, and associated symptoms.
What Is a Hernia?
A hernia occurs when an internal organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. This creates a noticeable bulge that becomes more prominent when standing, coughing, or straining.
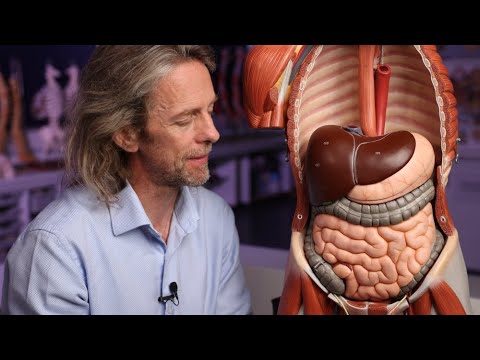
Hernias occur most commonly in the abdominal wall, where a portion of intestine or fat protrudes through weakened muscle. The three main types include:
- Inguinal hernias – located in the groin area
- Umbilical hernias – occur at the belly button
- Incisional hernias – develop at previous surgical sites
The abdomen contains the majority of hernias due to increased pressure from daily activities like lifting, coughing, or bowel movements. These hernias rarely heal on their own and typically worsen over time without treatment.
How Hernias Develop
Hernias form when muscle walls weaken and can no longer contain internal organs properly. Age increases hernia risk as muscles naturally lose strength and elasticity over time.
Several factors contribute to hernia development:
| Cause | Description |
|---|---|
| Birth defects | Congenital weakness in muscle walls |
| Previous surgery | Surgical incisions create weak points |
| Injury | Trauma that damages muscle tissue |
| Chronic strain | Repeated pressure from lifting or coughing |
The abdominal wall experiences constant pressure from internal organs, making it particularly susceptible to hernias. Pregnancy, obesity, and chronic constipation increase this pressure significantly.
Signs You May Need Hernia Repair
Most hernias require surgery when they cause pain, grow larger, or risk complications. A visible bulge that appears during physical activity often signals the need for medical evaluation.
Key symptoms indicating surgical repair may require immediate attention include:
- Severe pain or tenderness at the hernia site
- Nausea and vomiting accompanying hernia pain
- Inability to push the bulge back into the abdomen
- Skin discoloration around the hernia area
Strangulated hernias represent medical emergencies requiring immediate repair. This occurs when blood flow to herniated tissue becomes restricted, potentially causing tissue death.
Healthcare providers typically recommend surgery for hernias that interfere with daily activities or cause persistent discomfort. Early intervention prevents complications and generally results in better outcomes than waiting until emergency situations develop.
Types of Hernias That May Require Surgical Intervention
Most true hernias require surgical repair to prevent serious complications like incarceration or strangulation. Different types of hernias affect specific areas of the abdominal wall and present unique challenges for treatment.
Inguinal Hernia
Inguinal hernias represent the most common type of abdominal wall hernia, occurring when intestinal tissue pushes through a weak spot in the lower abdominal wall near the groin area. Men experience this condition more frequently than women due to anatomical differences in the inguinal canal.
The hernia typically appears as a visible bulge in the groin or scrotum area. Patients often report pain or discomfort that worsens with activities like lifting, coughing, or bending over.
Common symptoms include:
- Bulge in the groin that may disappear when lying down
- Sharp or burning pain at the bulge site
- Heavy sensation in the groin area
- Pain that increases with physical activity
Surgical repair remains the standard treatment for inguinal hernias. Surgeons can perform either open repair with a direct incision or minimally invasive laparoscopic surgery using small incisions and mesh reinforcement.
Umbilical Hernia
Umbilical hernias occur when tissue protrudes through the abdominal wall near the belly button. These hernias are particularly common in infants and may resolve naturally as abdominal muscles strengthen during the first few years of life.
Adult umbilical hernias typically result from increased abdominal pressure due to pregnancy, obesity, or fluid accumulation. Unlike pediatric cases, adult umbilical hernias require surgical intervention since they cannot heal independently.
The primary symptom involves a visible bulge near the navel that may increase in size when coughing, straining, or crying in infants. Adults may experience mild pain or discomfort around the belly button area.
Risk factors for adult umbilical hernias:
- Obesity
- Multiple pregnancies
- Previous abdominal surgery
- Chronic coughing or straining
Surgical repair involves pushing the protruding tissue back into place and closing the opening with sutures or mesh reinforcement to prevent recurrence.
Femoral and Incisional Hernias
Femoral hernias develop when tissue pushes through the femoral canal located just below the inguinal ligament in the upper thigh area. Women, particularly older women, experience femoral hernias more frequently than men due to anatomical differences in pelvic structure.
These hernias carry a higher risk of strangulation compared to other types. The narrow opening of the femoral canal can easily trap herniated tissue, cutting off blood supply and creating a surgical emergency.
Incisional hernias form at the site of previous surgical incisions when the abdominal wall fails to heal properly. These ventral hernias can occur months or years after the original surgery, particularly following procedures involving large abdominal incisions.
Factors that increase incisional hernia risk include surgical site infections, excessive strain on healing tissues, and incomplete wound closure. Patients typically notice a bulge near their surgical scar that may cause pain or discomfort.
Both femoral and incisional hernias require prompt surgical repair due to their high complication rates and inability to resolve without intervention.
Hiatal and Other Less Common Hernias
Hiatal hernias occur when part of the stomach pushes through the diaphragm into the chest cavity. Unlike other abdominal wall hernias, hiatal hernias often cause symptoms related to gastroesophageal reflux rather than visible bulging.
Patients with hiatal hernias frequently experience heartburn, acid reflux, difficulty swallowing, and chest discomfort. Small hiatal hernias may respond to medication and lifestyle changes, but larger ones typically require surgical repair.
Epigastric hernias develop in the upper abdomen between the navel and breastbone when fatty tissue pushes through weak spots in the abdominal muscles. These hernias appear as small lumps that may cause upper abdominal pain or tenderness.
Spigelian hernias represent a rare type of ventral hernia occurring along the edge of the rectus abdominis muscle. Their location beneath layers of fat and muscle makes them difficult to detect without imaging studies like ultrasound or CT scans.
All of these less common hernia types require surgical intervention since they cannot resolve naturally and may lead to complications if left untreated.
Hernia Repair Surgery: Procedures, Recovery, and Outcomes
Hernia repair surgery involves three main surgical approaches that address weakened abdominal walls through different techniques. Patients can expect a structured process from preparation through recovery, with most procedures completed as outpatient surgeries.
Surgical Repair Methods: Open, Laparoscopic, Robotic
Open surgery represents the traditional approach where surgeons create a single incision several inches long directly over the hernia site. This method provides direct access to repair the weakened abdominal wall and reposition herniated tissue.
Laparoscopic surgery offers a minimally invasive alternative using three to four small incisions, each approximately one inch long. Surgeons insert a tiny camera and specialized instruments to perform the repair with enhanced precision.
Robotic surgery utilizes advanced robotic systems to provide surgeons with improved dexterity and visualization during minimally invasive procedures. This approach typically requires longer operative time compared to open or laparoscopic methods.
Most hernia repair procedures incorporate surgical mesh to reinforce the weakened tissue and reduce recurrence rates. Surgeons may also use sutures to bring healthy tissue together, creating a stronger barrier wall around the repair site.
What to Expect Before, During, and After Surgery
Pre-surgical preparation includes medical history review, medication assessment, and necessary blood tests or imaging studies. Patients may need to discontinue blood-thinning medications and fast before surgery.
During the procedure, patients receive appropriate anesthesia – general anesthesia for laparoscopic approaches or local anesthesia for some open repairs. Surgery duration ranges from 30 minutes for simple repairs to five hours for complex abdominal wall reconstruction cases.
Post-operative recovery typically occurs in an outpatient setting with same-day discharge. Patients require arranged transportation home and should plan for 24 hours of rest following surgery.
Recovery involves gradual resumption of normal activities while following specific post-operative instructions. Most patients can perform basic activities like walking within the first day but must limit strenuous activities for several weeks.
Potential Risks and Complications
Hernia repair surgery carries standard surgical risks including infection, bleeding, and adverse reactions to anesthesia. These complications occur infrequently but require immediate medical attention when they develop.
Mesh-related complications may include chronic pain, mesh migration, or rejection of the synthetic material. Some patients experience temporary numbness or tingling around the incision sites.
Hernia recurrence remains a possibility, particularly in cases involving large hernias or patients with risk factors such as obesity or chronic coughing. Proper surgical technique and mesh reinforcement significantly reduce recurrence rates.
Patients should monitor for signs of complications including excessive pain, swelling, fever, or changes in bowel function. Most complications can be effectively managed when identified early through appropriate medical follow-up.
Prevention, Risk Factors, and Long-Term Hernia Management
Understanding hernia risk factors enables both prevention strategies and proper long-term management. Certain populations face higher risks due to structural weaknesses in connective tissue and abdominal muscles, while specific lifestyle modifications can reduce hernia development and recurrence rates.
Who Is at Risk for Hernias?
Age represents a primary risk factor as hernias are more common in older adults due to weakening abdominal muscles and connective tissue over time. Previous abdominal surgery creates significant risk, with incisional hernias developing in 2% to 20% of patients after open procedures.
Pregnant women face elevated risk from increased abdominal pressure and hormonal changes affecting connective tissue strength. Patients with gynecologic malignancies also show higher hernia rates due to complex surgical procedures and compromised healing.
High-Risk Conditions:
- Chronic cough or respiratory conditions
- Obesity and excessive weight
- Frequent heavy lifting
- Genetic connective tissue disorders
- Previous hernia repairs
Structural factors include birth defects and congenital weakness in muscle walls. Men develop inguinal hernias more frequently, while women show higher rates of femoral hernias. Patients with conditions impairing wound healing face substantially increased risk.
Preventative Measures and Lifestyle Considerations
Weight management reduces abdominal pressure on weakened muscle areas. Maintaining healthy body weight decreases strain on connective tissue and abdominal muscles that support internal organs.
Proper lifting techniques prevent sudden pressure increases. Hernia patients should lift with their legs, avoid twisting motions, and use supportive equipment when possible. Gradual strength building helps maintain muscle integrity.
Preventative Strategies:
- Control chronic coughing through medical treatment
- Avoid straining during bowel movements
- Strengthen core muscles gradually
- Maintain proper posture
- Use abdominal binders when recommended
Smoking cessation improves tissue healing and reduces chronic cough risk. Adequate nutrition supports connective tissue repair and maintains muscle strength. Patients should address constipation to prevent straining during bowel movements.
Recurrence and Follow-Up Care
Hernia recurrence rates vary by repair type and patient factors. Mesh repairs show lower recurrence rates compared to tissue-only repairs, though both approaches require proper surgical technique and post-operative care.
Pain management becomes crucial for long-term success. Chronic pain affects some patients following hernia repair, requiring specialized treatment approaches beyond standard recurrence prevention methods.
Follow-Up Requirements:
- Regular surgical site monitoring
- Activity restriction compliance
- Weight management maintenance
- Prompt reporting of new symptoms
Long-term monitoring identifies early recurrence signs including bulging, discomfort, or pain at previous repair sites. Patients should maintain communication with surgical teams and report changes promptly. Some individuals require multiple repairs over time, particularly those with connective tissue disorders or high-risk factors that cannot be completely modified.
Frequently Asked Questions
Patients commonly seek clarification about hernia types, symptoms, treatment approaches, and recovery expectations. Understanding these key aspects helps individuals make informed decisions about their care.
What are the different types of hernias that can occur?
Inguinal hernias develop in the groin area and represent the most common type, while umbilical hernias occur near the belly button. Hiatal hernias form when part of the stomach pushes through the diaphragm into the chest cavity. Incisional hernias develop at previous surgical sites where the abdominal wall has weakened.
How can I identify the signs and symptoms of a hernia?
A visible bulge or swelling in the affected area serves as the primary indicator of most hernias. Pain or discomfort may increase during physical activities like lifting, coughing, or straining. Some patients experience a burning sensation or feeling of heaviness in the hernia location.
Small hernias might not produce noticeable symptoms initially. Hiatal hernias often cause heartburn, chest pain, or difficulty swallowing rather than visible bulging.
What are the potential risks if a hernia is left untreated?
Most untreated hernias gradually increase in size over time without causing immediate danger. The primary concern involves potential strangulation, where blood supply to trapped tissue becomes restricted. This condition requires emergency surgical intervention to prevent tissue death.
Bowel obstruction can occur when intestinal contents become trapped within the hernia sac. While these serious complications remain relatively rare, they represent significant medical emergencies.
What treatment options are available for hernia repair?
Surgical repair remains the definitive treatment for most hernias requiring intervention. Laparoscopic techniques offer minimally invasive approaches with smaller incisions and faster recovery times. Open surgical methods provide direct access for complex cases or when laparoscopic repair proves unsuitable.
Surgical mesh reinforcement helps strengthen weakened tissue and reduces recurrence rates. Local anesthesia works for open repairs while laparoscopic procedures typically require general anesthesia.
How long is the recovery process after hernia surgery?
Initial recovery typically spans 1-2 weeks for routine activities, with full recovery taking 4-6 weeks. Minimally invasive laparoscopic procedures generally allow faster return to normal activities compared to open surgery. Patients can usually resume light work within a few days following laparoscopic repair.
Heavy lifting restrictions remain in place for several weeks post-surgery. Individual recovery times vary based on hernia size, surgical technique, and patient health factors.
Can lifestyle changes help in managing a hernia?
Weight management reduces abdominal pressure that can worsen existing hernias or contribute to new ones developing. Avoiding heavy lifting and straining helps prevent hernia progression and reduces discomfort. Proper lifting techniques using leg muscles rather than abdominal muscles provide protection.
Dietary modifications may help manage hiatal hernia symptoms by reducing acid reflux. However, lifestyle changes cannot cure existing hernias or eliminate the need for surgical repair when medically indicated.