Many women experience unexplained symptoms like irregular periods, unexpected weight gain, or excessive hair growth without realizing these could be signs of a common hormonal condition. Polycystic ovary syndrome affects up to 5 million women in the United States, yet more than half don’t know they have it.
PCOS can be identified through three main indicators: irregular or absent periods, elevated androgen levels causing excess hair growth or acne, and enlarged ovaries with multiple small cysts. The condition typically emerges around the time of first menstruation, though symptoms can develop years later. Since many PCOS symptoms overlap with other conditions, proper medical evaluation becomes essential for accurate diagnosis.
Understanding the full spectrum of PCOS symptoms, from obvious signs to subtle indicators, helps women recognize when to seek medical attention. Early identification allows for timely treatment that can address immediate concerns while preventing serious long-term health complications like diabetes and heart disease.
Recognizing PCOS: Key Signs and Symptoms
PCOS presents through four primary symptom categories that affect millions of women. These include menstrual irregularities, unexplained weight changes, altered hair growth patterns, and persistent skin issues.
Irregular Periods and Menstrual Changes
Irregular menstrual cycles serve as one of the most recognizable indicators of PCOS. Women with this condition often experience periods that occur less than eight times per year or cycles that extend beyond 35 days.
Some women may go months without menstruating at all. Others experience unpredictable bleeding patterns where periods arrive unexpectedly or last longer than normal.
Common menstrual irregularities include:
- Absent periods for three or more consecutive months
- Cycles longer than 35 days
- Fewer than eight periods annually
- Heavy or prolonged bleeding when periods do occur
These irregular cycles occur because elevated androgen levels disrupt normal ovulation. When ovulation becomes infrequent or stops entirely, the typical monthly hormonal fluctuations that trigger regular periods become disrupted.
Unexplained Weight Gain and Obesity
Weight gain represents another significant symptom of PCOS, particularly around the midsection. Many women notice they gain weight despite maintaining their usual diet and exercise habits.
This weight gain often proves resistant to traditional weight loss methods. The excess weight typically concentrates around the abdomen rather than distributing evenly throughout the body.
Weight-related symptoms include:
- Rapid weight gain without dietary changes
- Difficulty losing weight despite calorie restriction
- Increased abdominal fat accumulation
- Higher body mass index compared to family members
Insulin resistance frequently accompanies PCOS, making it harder for the body to process sugars effectively. This metabolic dysfunction contributes to both weight gain and difficulty maintaining a healthy weight.
Excess Hair Growth (Hirsutism) and Hair Loss
Hirsutism affects up to 70% of women with PCOS, causing thick, dark hair to grow in typically male patterns. This occurs due to elevated testosterone and other androgens circulating in the body.
Hair growth commonly appears on the face, particularly the chin and upper lip. Women may also notice increased hair on their chest, back, or inner thighs.
Areas where excess hair typically develops:
- Face (chin, upper lip, cheeks)
- Chest and breasts
- Lower abdomen
- Inner thighs and buttocks
Conversely, some women experience male-pattern hair loss on their scalp. Hair may thin at the crown or recede at the temples, similar to androgenic alopecia in men.
The combination of excess body hair and scalp hair loss creates a particularly distressing symptom profile that significantly impacts quality of life.
Persistent Acne and Skin Changes
Adult acne frequently persists or develops in women with PCOS due to excess androgen production. This acne often appears more severe than typical teenage breakouts and proves resistant to standard treatments.
The acne typically concentrates on the lower face, jawline, and neck. It may also appear on the chest and upper back areas.
Skin changes associated with PCOS:
- Deep, cystic acne lesions
- Oily skin texture
- Dark patches (acanthosis nigricans) on neck, armpits, or under breasts
- Slow healing of blemishes
Acanthosis nigricans creates dark, velvety patches of skin that commonly develop in body folds. These patches indicate insulin resistance and appear most frequently on the neck, armpits, and groin areas.
The combination of persistent acne and darkened skin patches often provides healthcare providers with important diagnostic clues when evaluating potential PCOS cases.
Other Common and Overlooked PCOS Symptoms
Many women with PCOS experience subtle symptoms that extend beyond reproductive issues. Mental health changes, skin darkening, and sleep disturbances often go unrecognized as PCOS-related symptoms.
Mood Swings, Anxiety, and Depression
Women with PCOS experience depression and anxiety at significantly higher rates than the general population. These mental health symptoms stem from the complex hormonal imbalance that characterizes the condition.
Hormonal fluctuations affect neurotransmitter production, particularly serotonin and dopamine. Low estrogen levels can disrupt mood regulation, while elevated androgens may contribute to emotional instability.
The psychological impact extends beyond biochemical changes:
- Body image concerns from physical symptoms like weight gain or hair loss
- Stress from fertility challenges and irregular menstrual cycles
- Social anxiety related to visible symptoms like acne or excess hair growth
Women often experience sudden mood swings that feel disproportionate to triggers. These emotional shifts can occur without warning and may intensify around menstrual periods.
Depression in PCOS frequently manifests as persistent fatigue, loss of interest in activities, and feelings of hopelessness. Many women report feeling emotionally “flat” or disconnected from their usual interests.
Skin Darkening (Acanthosis Nigricans)
Acanthosis nigricans appears as dark, velvety patches of skin that commonly develop in body folds. This condition affects up to 70% of women with PCOS and serves as a visible marker of insulin resistance.
The darkening typically occurs in these areas:
- Neck creases and back of neck
- Underarms and groin folds
- Knuckles and finger joints
- Elbows and knee creases
These patches develop when excess insulin triggers skin cell overgrowth. The affected areas may feel slightly thicker or rougher than surrounding skin.
Many women mistake acanthosis nigricans for poor hygiene or assume the darkening will fade with scrubbing. However, the condition requires addressing the underlying insulin resistance rather than topical treatments.
The severity often correlates with the degree of insulin resistance. Women who notice these patches should discuss metabolic testing with their healthcare provider.
Sleep Apnea and Persistent Fatigue
Sleep disturbances affect up to 70% of women with PCOS, with sleep apnea occurring five times more frequently than in women without the condition. Hormonal changes and weight distribution patterns contribute to airway obstruction during sleep.
Sleep apnea symptoms include:
- Loud snoring or gasping during sleep
- Morning headaches and dry mouth
- Difficulty concentrating during the day
- Witnessed breathing interruptions
The persistent fatigue in PCOS extends beyond typical tiredness. Women describe feeling exhausted despite adequate sleep hours, experiencing energy crashes throughout the day.
Multiple factors contribute to this overwhelming fatigue:
- Poor sleep quality from hormonal disruptions
- Blood sugar fluctuations causing energy dips
- Chronic inflammation depleting energy reserves
- Thyroid dysfunction often accompanying PCOS
This fatigue interferes with daily activities and work performance. Many women find themselves relying on caffeine or struggling to maintain their usual activity levels.
The combination of sleep apnea and hormonal imbalance creates a cycle where poor sleep worsens insulin resistance, which further disrupts sleep patterns.
Understanding PCOS Diagnosis and Medical Evaluation
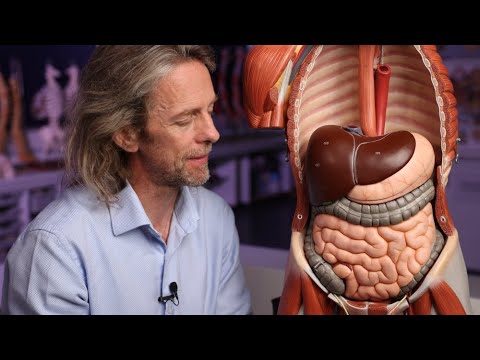
PCOS diagnosis requires meeting specific medical criteria established by international reproductive health organizations, with ultrasound imaging playing a crucial role in identifying polycystic ovaries. A gynecologist conducts a comprehensive evaluation combining physical examination, hormonal testing, and imaging studies to confirm the diagnosis.
Rotterdam Criteria and Diagnostic Tools
The Rotterdam Criteria serve as the most widely accepted diagnostic standard for polycystic ovary syndrome. Healthcare providers must identify at least two of three key features to confirm PCOS diagnosis.
The three diagnostic criteria include:
- Clinical or biochemical hyperandrogenism (excess male hormones)
- Oligo-anovulation (irregular or absent ovulation)
- Polycystic ovaries visible on ultrasound
Physicians also rule out other conditions that mimic PCOS symptoms. These include thyroid disorders, adrenal gland problems, and other hormonal imbalances.
Diagnostic testing typically involves blood work measuring hormone levels. Key tests include testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and anti-Müllerian hormone (AMH).
The LH to FSH ratio often appears elevated in women with PCOS. Normal ratios usually stay around 1:1, while PCOS patients frequently show ratios of 3:1 or higher.
Role of Ultrasound and Identifying Cysts
Ultrasound imaging provides essential visual confirmation of polycystic ovaries in PCOS diagnosis. Transvaginal ultrasound offers the clearest images of ovarian structure and follicle distribution.
Polycystic ovarian morphology appears on ultrasound as ovaries containing 12 or more follicles measuring 2-9mm in diameter. Alternatively, ovarian volume exceeding 10 mL³ in at least one ovary also indicates polycystic morphology.
These follicles are not true cysts but rather immature egg follicles that failed to develop properly. The “cysts” in polycystic ovaries represent arrested follicular development rather than pathological cyst formation.
Ultrasound timing matters for accurate results. The examination works best during the follicular phase of the menstrual cycle when possible. Women using hormonal contraception may need to discontinue use temporarily for accurate assessment.
Consulting a Gynecologist for Assessment
A gynecologist specializing in reproductive endocrinology provides the most comprehensive PCOS evaluation. These specialists understand the complex hormonal interactions and can differentiate PCOS from similar conditions.
The initial consultation includes a detailed medical history focusing on menstrual patterns, weight changes, and family history. Physical examination checks for signs of hyperandrogenism including hirsutism, acne, and male-pattern hair loss.
Ferriman-Gallwey scoring helps quantify hirsutism objectively. This system evaluates hair growth in nine body areas, scoring each from 0-4 based on terminal hair density.
Follow-up appointments allow monitoring of treatment response and symptom progression. Regular evaluation helps adjust treatment plans and screen for long-term complications like diabetes and cardiovascular disease.
Early diagnosis through proper medical evaluation enables timely intervention. This prevents progression to more serious complications while improving fertility outcomes and quality of life.
Potential Health Risks and Long-Term Impact of PCOS
PCOS significantly increases the risk of several serious health conditions including type 2 diabetes, cardiovascular disease, and endometrial cancer. Women with PCOS face a seven-fold higher risk of developing diabetes compared to those without the condition, while also experiencing elevated rates of heart disease and reproductive complications.
Infertility and Reproductive Health Concerns
Infertility affects approximately 70-80% of women with PCOS due to irregular or absent ovulation. The condition disrupts normal egg release, making conception difficult without medical intervention.
Women with PCOS often experience:
- Irregular menstrual cycles lasting longer than 35 days
- Complete absence of periods for months
- Difficulty conceiving naturally
Ovulation induction treatments can help restore fertility in many cases. However, women with PCOS who do conceive face higher risks of pregnancy complications.
Gestational diabetes occurs more frequently in pregnant women with PCOS. The risk increases particularly in obese women who required fertility treatments to conceive.
Miscarriage rates are also elevated among women with PCOS compared to the general population. Early pregnancy loss often relates to hormonal imbalances and insulin resistance associated with the condition.
Insulin Resistance and Risk of Diabetes
Insulin resistance affects up to 70% of women with PCOS, regardless of body weight. This condition occurs when cells become less responsive to insulin, forcing the pancreas to produce higher amounts.
The progression to type 2 diabetes happens rapidly in women with PCOS. Research shows that 25-30% of women with PCOS develop impaired glucose tolerance by age 30.
Key diabetes risk factors include:
- Central obesity and abdominal fat distribution
- Family history of diabetes
- Sedentary lifestyle
- Age over 30
Women with PCOS show a seven-fold increased risk of developing type 2 diabetes compared to women without the condition. This risk remains elevated even in non-obese women with PCOS.
Early detection through regular glucose testing allows for preventive interventions. Lifestyle modifications including diet changes and exercise can significantly reduce diabetes risk in women with PCOS.
Heart Disease, High Blood Pressure, and Cholesterol
Cardiovascular disease risk increases substantially in women with PCOS due to multiple interconnected factors. Insulin resistance directly contributes to arterial damage and atherosclerosis development.
Women with PCOS typically exhibit concerning lipid profiles:
- Elevated triglycerides
- High LDL cholesterol
- Low HDL cholesterol
- Increased inflammatory markers
High blood pressure occurs three times more frequently in women with PCOS aged 40-59 compared to controls. The relationship between insulin levels and blood pressure appears direct and significant.
Coronary artery disease shows greater severity in women with PCOS when examined through angiography. These women develop atherosclerotic conditions at younger ages than their peers.
Stroke risk increases due to the combination of high blood pressure, abnormal cholesterol levels, and increased clotting factors. Elevated plasminogen activator inhibitor-1 levels impair the body’s natural clot-dissolving mechanisms.
Increased Risk of Endometrial Cancer
Endometrial cancer risk increases significantly in women with PCOS due to prolonged exposure to unopposed estrogen. Chronic anovulation prevents progesterone production, which normally protects the uterine lining.
Endometrial hyperplasia serves as a precursor to cancer in many cases. Studies indicate that 18% of adenomatous hyperplasia cases progress to cancer within 2-10 years.
Women with PCOS face a 3.1-fold increased risk of endometrial cancer according to large-scale studies. This risk correlates directly with the frequency and duration of menstrual irregularities.
Menstrual intervals exceeding three months may indicate endometrial hyperplasia development. Regular monitoring becomes essential for early detection and prevention.
Risk factors that compound endometrial cancer danger include:
- Obesity
- Nulliparity (never giving birth)
- Diabetes
- Prolonged anovulation
Regular gynecological examinations and endometrial assessments help detect abnormal changes early when treatment remains most effective.
Frequently Asked Questions
Women experiencing irregular periods, weight changes, or unusual hair growth patterns often have questions about PCOS diagnosis and its effects on their health. These concerns typically center around identifying symptoms, understanding metabolic impacts, and recognizing reproductive complications.
What are the common symptoms associated with Polycystic Ovary Syndrome (PCOS)?
PCOS typically presents with irregular menstrual periods, excess facial or body hair growth, acne, weight gain, and difficulty conceiving.
How do irregular periods relate to a possible diagnosis of PCOS?
Irregular periods involving fewer than nine cycles per year or periods occurring more than 35 days apart are key diagnostic indicators of PCOS.
Can weight gain or difficulty losing weight be indicative of PCOS?
Weight gain and difficulty losing weight often occur with PCOS due to insulin resistance, which affects how the body processes sugar and stores fat.
Are there any specific signs of PCOS that appear on the skin or hair?
PCOS commonly causes excess facial and body hair growth, severe acne, male-pattern baldness, and dark patches of skin on the neck, armpits, or groin areas.
What reproductive complications might suggest the presence of PCOS?
PCOS frequently leads to infertility, irregular ovulation, increased miscarriage risk, and complications during pregnancy including gestational diabetes.
How does PCOS affect overall metabolism and long-term health risks?
PCOS increases the risk of developing type 2 diabetes, high blood pressure, heart disease, sleep apnea, and metabolic syndrome due to hormonal imbalances.