At Local MD, we believe that strong public health begins in the neighbourhood — and the beating heart of that neighbourhood care is primary care clinics. These clinics do far more than treat individual patients: they connect with families, communities and public-health systems to deliver prevention, education, early detection, and population-level impact. In this deep dive article, we explore how primary care clinics enhance public health across multiple dimensions, why they are indispensable for building healthy communities, and how we at Local MD bring these principles into practice.
The Central Role of Primary Care in Public Health
Primary care is defined by the World Health Organization (WHO) as the first point of contact, accessible and comprehensive, and tied to the broader concept of primary health care (PHC) which includes prevention, health promotion, treatment, rehabilitation and palliative care.
It is, as WHO says, “a whole-of-society approach to effectively organize and strengthen national health systems to bring services for health and wellbeing closer to communities.”
In simpler terms: primary care clinics sit at the intersection of personal health and community health. They are uniquely positioned to influence public-health outcomes by virtue of their accessibility, continuity, and ability to address the determinants of health, beyond just disease.
Key features of primary care in this regard include:
-
First-contact accessibility: People come to primary care clinics for all kinds of health concerns — not just emergencies. This gives an early opportunity for detection and prevention.
-
Continuity and relationships: Over time, a primary care clinic builds trust and rapport with patients and families, which is foundational for effective public-health work (screenings, lifestyle counselling, vaccination adherence).
-
Coordination of care: These clinics connect patients to other parts of the health system — specialists, hospitals, public-health services — ensuring that individuals don’t fall through the cracks.
-
Comprehensiveness: They provide a broad range of services — from prevention and health promotion to chronic-disease management and acute care — which means they can impact many public-health fronts.
Thus, primary care clinics are not just “mini hospitals” for everyday care — they are public-health engines at the grassroots level.
Ways Primary Care Clinics Promote Public Health
Preventive Services & Health Promotion
Prevention is the cornerstone of public health. Primary care clinics promote it through screening programs (e.g., blood pressure, cholesterol, diabetes risk), vaccinations, lifestyle counselling (smoking cessation, exercise, nutrition), and health education. At Local MD, our clinicians actively integrate prevention into each visit — not only treating symptoms but asking “What can we prevent next?”
By delivering preventive services systematically, these clinics reduce the incidence of disease, lower healthcare costs, and improve population health markers. They also reinforce the notion that health is more than absence of disease — it’s active maintenance of wellness.
Early Detection of Disease & Risk-Factor Management
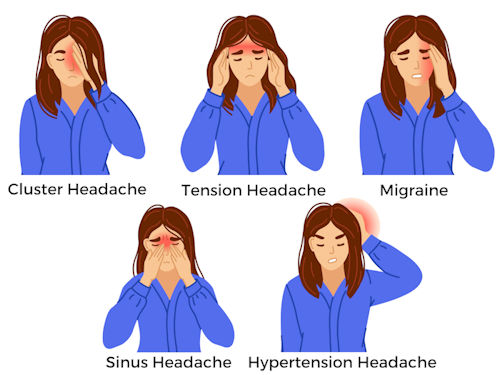
Primary care clinics are in a prime position to detect chronic disease or risk factors early — when interventions are more effective. For example:
-
An asymptomatic patient may get a screening blood pressure reading, prompting early hypertension management.
-
Routine counselling may identify pre-diabetes and allow lifestyle interventions before full-blown diabetes develops.
-
A well-woman exam or health check might identify early signs of reproductive health issues.
These early detections matter not just for the individual but for public health: fewer complications, less advanced disease burden, and reduced strain on the health-system. Primary care providers thus act not only as healers but as guardians of the community’s health.
Chronic Disease Management & Reducing Health Disparities
Chronic diseases (e.g., hypertension, diabetes, obesity, asthma) are major public-health burdens. Primary care clinics provide longitudinal care for these conditions — supporting adherence, monitoring complications, and educating patients. By doing so, they reduce avoidable hospitalizations and improve quality of life.
Importantly, they also serve to reduce health disparities. Accessible primary care in underserved communities helps ensure that vulnerable populations receive timely care, thereby bridging gaps in outcomes. Clinics like Local MD, when oriented to community needs, can target high-risk groups and deliver care that is culturally competent and locally relevant.
Vaccination & Infectious Disease Control
Primary care clinics support immunization campaigns (routine childhood vaccines, adult boosters, seasonal flu, COVID-19), which are core public-health activities. They also play a role in infectious-disease surveillance — identifying and reporting cases, educating patients about infection prevention, and coordinating with public-health authorities.
By being embedded in the community, primary care clinics help control outbreaks and minimize infectious-disease spread — a foundational public-health function.
Community Outreach, Health Literacy & Empowerment
Health literacy is crucial. Primary care clinics enable outreach — group education sessions, workshops, collaboration with community organisations. They empower individuals to take charge of their health: understand screenings, adopt healthier behaviours, adhere to medications. When local clinics root themselves in community networks, they become trusted avenues for health information and behaviour change. Primary-care efforts in health promotion link directly to public-health improvement.
Data Collection, Surveillance & Referrals to Public Health Systems
While individual clinic visits are focused on patients, each interaction generates data — about screenings, risk factors, disease prevalence, vaccination rates. Primary care clinics feed this data into broader public-health monitoring. They help identify emerging trends (e.g., rising diabetes in a neighborhood), support local health-planning (targeting high-risk zones), and trigger public-health interventions.
Moreover, they coordinate referrals to specialist services or hospital care when needed — ensuring seamless care pathways and avoiding delays.
Addressing Social Determinants of Health & Community Integration
Health outcomes are not determined purely by clinical care — social determinants (income, education, environment, food security) matter greatly. Primary care clinics that engage with these dimensions (through social-work support, dietary counsellors, community partnerships) extend public-health impact beyond the exam room. They may collaborate with local agencies to promote healthy housing, nutritious food access, smoking cessation in the community, or elder-care support. This holistic orientation strengthens community health.
Why Local Communities Especially Benefit from Primary Care Clinics
-
Accessibility: Clinics located within neighbourhoods reduce travel, waiting time and cost barriers — meaning people access care earlier and more often.
-
Trust & Continuity: In many communities, having a reliable familiar clinic fosters trust, which leads to higher uptake of preventive services and improved outcomes.
-
Tailored to Local Needs: Community-based clinics can adapt services to local epidemiology, culture and language, making public-health efforts more effective.
-
Cost-Effectiveness: Strong primary care has been shown to reduce overall health-system costs by reducing emergency visits, hospitalisations and late-stage disease care.
-
Equity: Primary care clinics help serve underserved populations, reduce health inequities and promote health justice.
How Local MD Implements Public-Health-Oriented Primary Care
At Local MD, our approach is rooted in the integration of clinical care and community-oriented public health. Here’s how we bring the above principles to life:
-
We design our clinic services to include prevention and screenings as standard parts of every visit, not optional add-ons.
-
We maintain community outreach programmes: health fairs, vaccination drives, educational workshops and partnerships with local organisations.
-
We embed data monitoring — tracking local population health metrics, screening uptake, chronic-disease control, and feeding insights back into our strategy.
-
We train our team not only in clinical care but in behaviour change, health coaching and culturally sensitive communication.
-
We coordinate with public-health agencies to support vaccination campaigns, outbreak surveillance and referral networks.
-
We ensure accessibility — flexible hours, sliding scale payment, telehealth options — to reach the widest possible segment of the community.
-
We engage with community stakeholders — schools, churches, community centres — to leverage trusted local networks for health messaging and intervention.
Challenges & Considerations in Maximizing Public Health Impact
While primary care clinics hold huge potential, several challenges must be addressed:
-
Capacity & Resources: Clinics must be adequately staffed and resourced to deliver both individual care and community health activities.
-
Integration with Public Health Systems: Effective linkage with municipal/state public-health agencies is crucial for data sharing, outbreak response, and population-level planning.
-
Health Literacy & Engagement: Reaching populations with low health literacy or mistrust of the system remains a challenge. Clinics must invest in communication and community trust-building.
-
Scope of Services: Balancing the demands of acute care, chronic-disease management, and public-health outreach can strain clinic workflows.
-
Measuring Impact: Public-health outcomes often accrue over long periods (e.g., reduced diabetes incidence) making it harder to track immediate ROI. Yet measurement is essential to justify investment and refine strategy.
-
Social Determinants of Health: Clinics can’t address all external determinants (poverty, housing, food security) alone — they must form partnerships and advocate for broader change.
Looking Ahead: The Future of Primary Care + Public Health
The future promises even more synergy between primary care clinics and public health:
-
Value-based care models are increasingly rewarding clinics that keep populations healthy rather than simply treating illness.
-
Digital health and telemedicine open new channels for outreach, monitoring and prevention even in underserved areas.
-
Community health worker integration is growing — bridging clinic care with community networks and social-services support.
-
Data analytics and population-health management tools allow clinics to stratify risk, target interventions and measure community impact more precisely.
-
Multi-sector collaboration — linking health clinics with education, housing, transportation, food systems — is strengthening the social-determinant dimension of public health.
For Local MD, we see primary care clinics as public-health hubs of the future — not only treating sickness but creating health, preventing disease, fostering resilience and building healthier communities.
Conclusion: Building Healthier Communities Through Primary Care
In summary, primary care clinics are foundational to public health in local communities. They provide accessible, continuous, coordinated and comprehensive care — and in doing so, they deliver prevention, early detection, health promotion, chronic-disease management and community empowerment. At Local MD, we champion this model because we believe that strong clinics mean strong communities.
Every visit to a primary care clinic is an opportunity — to not just treat illness, but to ask, “How can we keep you healthier tomorrow, next year, and for life?” That mindset, combined with community-oriented outreach and data-driven public-health collaboration, is what enables primary care clinics to fulfil their public-health promise.
If you are part of a community seeking stronger preventive health, better access, reduced disease burden and empowered citizens, look to your local primary care clinic as a vital partner. At Local MD, we are committed to being that partner — translating clinical care into community wellness and making public health local, personal and effective.