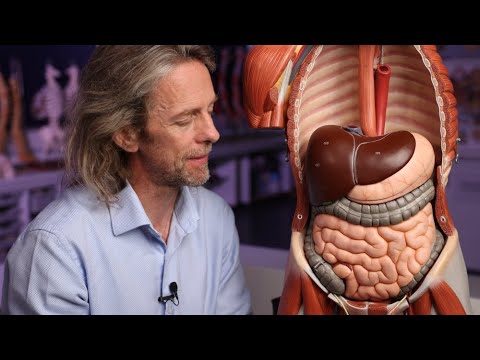
Obesity is a complex and chronic health condition affecting millions of people worldwide. Beyond concerns about weight itself, obesity significantly increases the risk of developing other serious health issues, including type 2 diabetes, high blood pressure, heart disease, and sleep apnea. Treating obesity is about more than shedding pounds—it’s about improving long-term health outcomes and reducing the burden of related chronic conditions. One important tool in the fight against obesity is oral weight loss medications. But how do these medications fit into managing obesity and its many complications?
At Local MD (https://www.localmd.nyc/), preventive care and individualized treatment plans are central to improving patient outcomes. In this article, we’ll explore the role oral weight loss medications play in managing obesity-related chronic conditions, how they work, who may benefit, and what considerations patients should keep in mind.
Understanding Obesity and Its Impact
Obesity is not simply a matter of willpower. It’s a medical condition influenced by factors such as genetics, metabolism, behavior, and environment. A Body Mass Index (BMI) of 30 or higher is typically classified as obese, though BMI isn’t the only measure clinicians use to assess health risk.
Obesity increases the risk of many chronic conditions:
-
Type 2 diabetes
-
Hypertension (high blood pressure)
-
Cardiovascular disease
-
Fatty liver disease
-
Certain types of cancer
-
Sleep apnea
-
Joint problems
Each of these conditions can independently reduce quality of life and increase long-term healthcare needs. Effectively managing obesity can, therefore, have cascading benefits across multiple organ systems.
What Are Oral Weight Loss Medications?
Oral weight loss medications are FDA-approved prescriptions designed to help individuals lose weight and maintain that loss as part of a broader treatment plan. Unlike over-the-counter supplements, these medications have been clinically tested for safety and effectiveness.
These medications can support weight loss in several ways:
-
Appetite Suppression: Reducing feelings of hunger to decrease caloric intake.
-
Metabolic Modulation: Affecting how the body processes sugars and fats.
-
Glycemic Control: Helping stabilize blood sugar, which is particularly useful for patients with insulin resistance or diabetes.
They are usually prescribed alongside lifestyle interventions, such as diet modification, physical activity, and behavioral counseling, because no medication alone can resolve obesity.
How Oral Weight Loss Medications Work
Different medications have different mechanisms of action. Some of the most common ways oral weight loss medications help include:
Appetite Regulation
Certain medications work on brain chemicals that influence hunger and satiety. By reducing appetite or increasing feelings of fullness, these drugs help patients stick to reduced-calorie diets with less discomfort.
Glycemic Management
Many individuals with obesity also struggle with insulin resistance. By improving blood glucose control, some weight loss medications can make it easier for patients to manage both weight and metabolic dysfunction.
Slowing Fat Absorption
Some medications reduce the amount of fat absorbed from food, which can contribute to weight loss, though this approach tends to be less common with oral prescriptions.
At Local MD, clinicians customize medication plans based on each patient’s health history, lifestyle, and goals. A tailored plan ensures both safety and effectiveness.
Who Can Benefit from Oral Weight Loss Medications?
Oral weight loss medications are typically considered for adults with:
-
A BMI ≥ 30 (classified as obese)
-
A BMI ≥ 27 with at least one obesity-related chronic condition (e.g., type 2 diabetes, hypertension)
These guidelines help clinicians weigh the potential benefits and risks of medication therapy.
However, medications are not appropriate for everyone. Patients with certain health conditions or those taking medications that might interact negatively may need alternative strategies. A thorough evaluation by a healthcare provider is essential.
Common Oral Weight Loss Medications
Here are some of the most widely used oral medications in the management of obesity:
1. Orlistat
Orlistat reduces fat absorption by inhibiting digestive enzymes in the gut. It’s been available for years and is generally well-tolerated, though it can cause gastrointestinal side effects.
2. Phentermine-Topiramate Combination
This medication combines an appetite suppressant with a drug that enhances satiety. Many patients experience meaningful weight loss with this therapy, but it must be monitored due to possible side effects.
3. Naltrexone-Bupropion Combination
This medication affects pathways in the brain that regulate hunger and cravings. It has shown positive results in weight management, especially when combined with lifestyle changes.
Each of these medications is approved by the U.S. Food and Drug Administration (FDA) for long-term weight management under clinical supervision.
Oral Weight Loss Medications and Chronic Conditions
Oral weight loss medications are not a cure-all—but they can significantly impact obesity-related chronic conditions when used appropriately.
Improved Glycemic Control
For patients with type 2 diabetes or prediabetes, weight loss can improve insulin sensitivity. Medications that help patients lose weight can reduce dependence on other diabetes medications and improve blood sugar levels.
Blood Pressure Reduction
Weight loss often leads to lower blood pressure. Even a modest reduction in weight can make a meaningful difference in cardiovascular risk.
Better Lipid Profiles
Losing excess weight often improves cholesterol levels, reducing the risk of heart disease and stroke.
Relief from Joint Pain and Sleep Apnea
Weight loss reduces stress on joints, improving mobility and pain levels. For individuals with sleep apnea, weight reduction can improve breathing during sleep and overall sleep quality.
Reducing obesity-related disease burden doesn’t just improve physical health—it enhances emotional well-being and quality of life.
Risks and Considerations
Like all medications, oral weight loss drugs come with potential side effects and risks. Common issues can include:
-
Nausea
-
Headache
-
Gastrointestinal discomfort
-
Elevated heart rate (with some medications)
Because of these risks, clinicians at Local MD conduct a thorough evaluation before prescribing medication. Patients with heart disease, uncontrolled hypertension, or specific genetic conditions may require additional monitoring or alternative strategies.
Women who are pregnant, planning pregnancy, or breastfeeding should generally avoid weight loss medications due to potential risks to the fetus or infant.
Integrating Medications with Lifestyle Changes
Oral weight loss medications work best when integrated with lifestyle interventions. These include:
Nutritional Counseling
Healthy eating patterns, portion control, and mindful eating are essential for long-term success.
Physical Activity
Regular exercise supports metabolic health, muscle strength, and cardiovascular fitness.
Behavior Modification
Addressing emotional eating, stress, and habits that contribute to weight gain helps patients establish sustainable lifestyle patterns.
A multidisciplinary approach ensures that patients build the skills needed for long-term weight management—even after medication is discontinued.
Monitoring and Follow-Up
Regular follow-up is a key part of effective treatment. During follow-up visits, healthcare providers may:
-
Track weight and vital signs
-
Assess medication effectiveness
-
Monitor for side effects
-
Adjust therapy as needed
Ongoing support improves adherence and helps patients navigate challenges throughout their weight management journey.
Myths About Oral Weight Loss Medications
Despite their proven benefits, misconceptions persist. Let’s address some common myths:
Myth 1: “Medications will make me lose weight without effort.”
Fact: Medications support weight loss but must be paired with lifestyle changes.
Myth 2: “Weight regain is impossible once I start medication.”
Fact: Long-term success depends on sustainable habits, even with medication.
Myth 3: “All weight loss medications are unsafe.”
Fact: FDA-approved medications are evaluated rigorously for safety and efficacy.
Understanding the facts empowers patients to make informed decisions about their treatment.
Who Should Avoid Oral Weight Loss Medications?
Not everyone is a good candidate for these medications. Individuals with certain conditions—including severe heart disease, uncontrolled high blood pressure, or certain psychiatric conditions—may need alternative strategies. Pregnant or breastfeeding women are typically advised to avoid weight loss medications.
A comprehensive evaluation by a clinician determines the safest, most effective approach for each individual.
Oral Weight Loss Medications and Long-Term Success
Weight loss is not just about short-term results. Long-term success involves:
-
Sustainable lifestyle changes
-
Continued medical support
-
Regular health screenings
-
Emotional and behavioral support
Medications can jump-start progress or help break plateaus, but lasting success is rooted in overall health behaviors.
Conclusion
Obesity is a chronic condition with far-reaching impacts on physical and mental health. Oral weight loss medications provide a valuable tool in managing obesity and its related chronic conditions when used appropriately and in combination with lifestyle changes.
At Local MD, personalized care helps patients navigate weight management with clinical expertise and supportive resources. From medication planning to nutritional guidance and ongoing follow-up, a comprehensive approach increases the likelihood of lasting success.
If you’re considering weight loss medications as part of your health plan, talk to your healthcare provider to determine the best strategy for your needs. Improved health is not just about a number on the scale—it’s about enhancing quality of life, reducing disease risk, and achieving long-term wellness.