Headaches affect millions of people worldwide, ranging from mild discomfort to debilitating pain that disrupts daily activities. While occasional headaches are common, recurring or severe headaches warrant attention and proper medical evaluation. Primary care physicians are often the first line of defense in diagnosing and treating headache disorders, with studies showing that over 90% of headache cases can be effectively managed through primary care interventions.
Many factors can trigger headaches, including stress, dehydration, lack of sleep, certain foods, and environmental stimuli. Understanding these triggers is crucial for developing an effective treatment plan. Primary care providers can help identify patterns through comprehensive health assessments and recommend appropriate lifestyle modifications or medications.
Seeking help for persistent headaches isn’t just about pain relief—it’s about improving quality of life and preventing potential complications. A visit to a primary care physician can determine whether headaches are primary (like tension or migraine headaches) or secondary (resulting from underlying conditions that may require specialized care).
Understanding Headache Types
Headaches manifest in different forms, each with distinct symptoms, triggers, and treatment approaches. Identifying the specific type of headache you experience is crucial for developing an effective management plan with your primary care provider.
Tension Headaches
Tension headaches are the most common type, affecting up to 80% of adults. They typically present as a dull, aching pain or pressure around the forehead, temples, or back of the head and neck.
These headaches often develop gradually and can last from 30 minutes to several days. Many patients describe the sensation as having a tight band wrapped around their head.
Migraine Headaches
Migraines affect approximately 12% of the population and are characterized by moderate to severe throbbing pain, typically on one side of the head. They can last from 4 hours to 3 days if untreated.
Common migraine symptoms:
- Pulsating or throbbing pain
- Nausea or vomiting
- Sensitivity to light and sound
- Visual disturbances (aura) in some cases
Many migraine sufferers experience warning signs hours or days before an attack, known as prodrome. These may include mood changes, food cravings, or increased yawning.
Triggers vary widely but often include hormonal changes, certain foods, stress, and environmental factors. Treatment options range from preventive medications to lifestyle modifications and acute pain relief.
Cluster Headaches
Cluster headaches are relatively rare but extremely painful headaches that occur in cyclical patterns or clusters. They cause severe, burning pain around or behind one eye.
These headaches can wake patients from sleep and typically last 15 minutes to 3 hours, recurring 1-8 times daily during a cluster period. Men are more commonly affected than women.
Key characteristics:
- Intense, one-sided pain
- Redness or tearing of the affected eye
- Nasal congestion or runny nose on the affected side
- Restlessness during attacks
Cluster periods may last weeks or months, followed by remission periods. Treatment focuses on stopping individual headaches quickly and preventing future episodes with oxygen therapy, triptans, or preventive medications.
Sinus Headaches
Sinus headaches result from inflammation in the sinus cavities, usually due to infection or allergies. They typically cause pain and pressure around the eyes, cheeks, and forehead.
The pain often worsens when bending forward or lying down. Many patients report increased pain in the morning due to mucus accumulation during sleep.
True sinus headaches are frequently accompanied by other symptoms:
- Nasal congestion or discharge
- Facial tenderness or swelling
- Fever (in cases of infection)
- Decreased sense of smell
It’s important to note that many self-diagnosed “sinus headaches” are actually migraines. Treatment targets the underlying cause with antibiotics for bacterial infections, decongestants, antihistamines, or nasal steroids.
Common Causes of Headaches
Headaches stem from various sources, ranging from everyday lifestyle factors to underlying medical conditions and even medication use patterns.
Lifestyle Triggers
Poor sleep patterns significantly contribute to headache frequency and intensity. Adults who regularly get less than 7 hours of sleep often experience more tension headaches and migraines.
Stress and tension rank among the most common headache triggers. When stress levels rise, muscles in the neck and scalp tighten, leading to pain that can radiate across the head.
Diet plays a crucial role in headache management. Common dietary triggers include:
- Caffeine (both consumption and withdrawal)
- Alcohol, especially red wine and beer
- Aged cheeses and processed meats
- Foods containing MSG or artificial sweeteners
Environmental factors such as bright lights, strong smells, and weather changes can provoke headaches in susceptible individuals.
Medical Conditions
Migraines affect approximately 12% of the population and typically present as throbbing pain on one side of the head. These headaches often come with nausea, sensitivity to light and sound, and sometimes visual disturbances called auras.
Sinus infections cause pain and pressure around the eyes, cheeks, and forehead. The pain typically worsens when bending forward or lying down.
Medication Overuse
Rebound headaches occur when pain medications are taken too frequently. Using over-the-counter pain relievers more than 15 days per month can paradoxically increase headache frequency.
The cycle works like this: A person takes pain medication for headache relief, but when the medication wears off, the headache returns, often worse than before. This leads to more medication use, creating a difficult-to-break pattern.
Common medications associated with rebound headaches include:
- Acetaminophen (Tylenol)
- Aspirin and ibuprofen (Advil, Motrin)
- Combination pain relievers containing caffeine
- Triptans and other prescription migraine medications
Breaking this cycle typically requires medical supervision. Gradual withdrawal from the overused medication combined with preventive therapies offers the best chance of resolution.
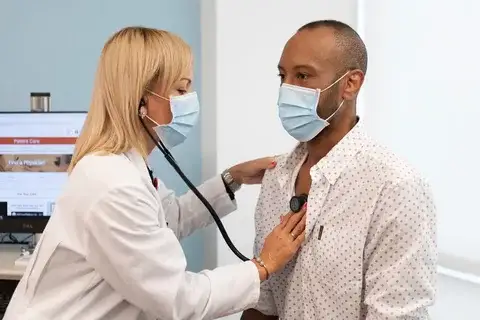
Primary Care Approaches for Headache Management
Primary care providers offer comprehensive approaches to manage headaches through proper diagnosis, individualized treatment plans, and effective prevention strategies. These methods address both immediate pain relief and long-term management to improve quality of life.
Accurate Diagnosis by Primary Care Providers
Primary care physicians employ several diagnostic tools to identify headache types and underlying causes. The process typically begins with a detailed medical history and symptom analysis.
Key diagnostic components include:
- Physical examinations focusing on neurological signs
- Headache diaries tracking frequency, duration, and triggers
- Standardized assessment tools like the Migraine Disability Assessment (MIDAS)
When necessary, providers may order imaging studies such as CT scans or MRIs to rule out serious conditions. Blood tests can help identify systemic issues like infections or hormonal imbalances that might contribute to headaches.
The diagnostic process also considers lifestyle factors and environmental triggers that may exacerbate symptoms. This comprehensive approach ensures treatment addresses the specific headache type rather than just symptom management.
Preventative Strategies
Prevention forms a cornerstone of effective headache management in primary care. Providers help patients identify and address personal triggers through detailed headache journals and lifestyle analysis.
Common preventative recommendations include:
- Maintaining regular sleep schedules
- Staying adequately hydrated
- Practicing stress reduction techniques like meditation
- Following consistent meal times to avoid blood sugar fluctuations
Exercise regimens tailored to patient capabilities can reduce headache frequency. Even moderate physical activity for 30 minutes several times weekly may decrease headache occurrence.
When to Seek Further Medical Attention
While most headaches are benign and resolve on their own, certain symptoms warrant prompt medical evaluation. Recognizing these warning signs can be crucial for your health and wellbeing.
Warning Signs of Serious Causes
Headaches that come on suddenly and feel like the “worst headache of your life” require immediate emergency care. This could indicate a brain hemorrhage or other serious condition.
Seek immediate medical attention if your headache is accompanied by fever, stiff neck, confusion, seizures, double vision, or weakness in any limb. These symptoms might suggest meningitis or a stroke.
New headaches that begin after age 50 or headaches that wake you from sleep should prompt a doctor’s visit. These patterns sometimes indicate underlying issues requiring investigation.
Critical red flags that require emergency evaluation:
- Headache following head trauma
- Headache with neurological changes
- Progressive worsening over days
- Headache during pregnancy or postpartum
Frequently Asked Questions
Headache and migraine sufferers often have specific concerns about their conditions that require clear, medical explanations. Understanding triggers, treatments, and management strategies can significantly improve quality of life for those dealing with chronic head pain.
What factors contribute to triggering migraines in women?
Hormonal fluctuations play a significant role in triggering migraines in women, particularly during menstruation, pregnancy, and menopause. Estrogen level changes can directly affect blood vessels and pain pathways in the brain.
Can migraines be fully eradicated with treatment?
Treatment success varies based on individual factors including migraine type, duration of condition, and genetic predisposition. Regular follow-ups with healthcare providers allow for treatment adjustments as needed.
What are the potential risks associated with frequent migraines?
Frequent migraines often lead to medication overuse headaches, creating a difficult cycle to break. Depression and anxiety disorders occur at higher rates among chronic migraine sufferers.
What immediate steps can one take for relief during a severe migraine attack?
Finding a dark, quiet room and applying cold compresses to the forehead or neck can provide immediate relief. Rest is essential, as movement typically worsens migraine pain and associated symptoms.
What are the typical causes of recurring headaches in men?
Work-related stress and poor ergonomics contribute significantly to tension headaches in men. Improper desk setups and prolonged screen time create neck and shoulder tension that radiates to the head.
How can chronic headaches be effectively managed with new medical approaches?
CGRP antagonists represent a breakthrough in migraine prevention, targeting specific pain pathways with fewer side effects than older medications. Monthly injections or daily oral options provide sustained relief for many patients previously resistant to treatmen