At Local MD, we recognise that safeguarding women’s health is a cornerstone of preventive care—as is protecting the next generation. One vaccine stands out as both a personal shield and a public-health imperative for women of reproductive age: the vaccine against Rubella. In this article, we explore why the rubella vaccine is crucial for women of childbearing age, how it works, and what steps you should take.
Understanding Rubella: More Than a Mild Childhood Illness
While rubella is often considered a “mild” viral illness in children—featuring a rash, low fever, and mild illness—its stakes change dramatically when the infection occurs during pregnancy. According to the Centers for Disease Control and Prevention (CDC), if a woman contracts rubella during early pregnancy, the virus can cross the placenta and cause devastating outcomes for the developing fetus.
This foetal impact is known as Congenital Rubella Syndrome (CRS) and may include birth defects such as hearing impairment, cataracts, heart defects, developmental delays, and even miscarriage or stillbirth. In short: what may seem benign for an adult is highly dangerous in the context of pregnancy.
Why Women of Childbearing Age Must Prioritise Rubella Immunity
Protecting the Unborn Child
The most compelling reason for vaccination is to prevent fetal harm. When a woman contracts rubella in her first trimester, the risk of CRS is highest. The CDC warns: “Rubella is very dangerous during pregnancy.” By receiving the vaccine before pregnancy, women can significantly reduce the risk of exposing their unborn child to rubella virus.
Lifelong Immunity and Elimination Efforts
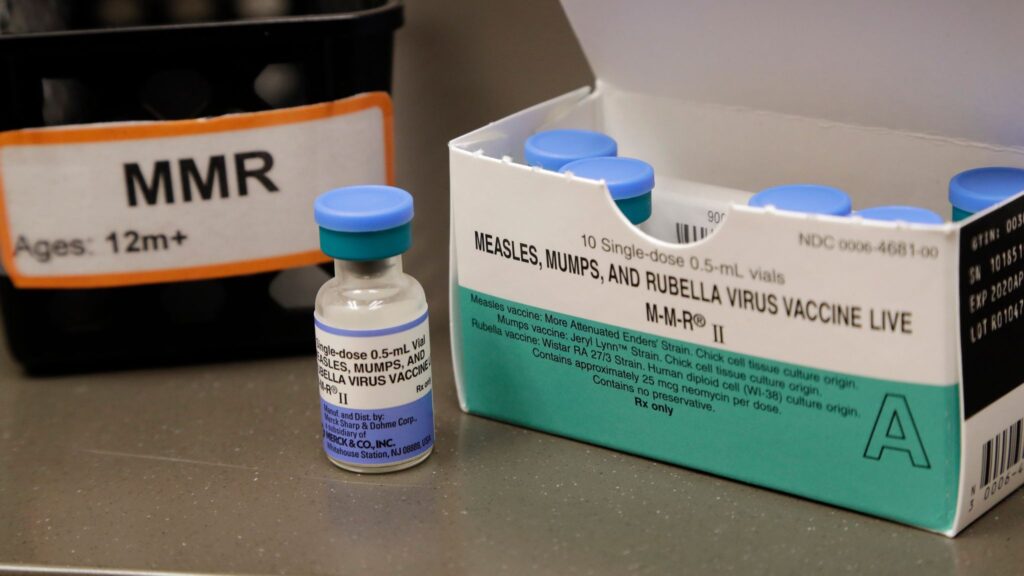
The rubella-containing vaccine—usually delivered as part of the measles–mumps–rubella (MMR) vaccine—offers very high protection, with immunity that often lasts a lifetime. Ensuring that all women of reproductive age are immune contributes to herd immunity and helps maintain elimination of rubella transmission in communities.
Avoiding Uncertainty During Pregnancy
Many women of childbearing age may be unaware of their immune status or whether they received rubella immunization. Formal documentation of immunity is advised. Being proactive avoids the scenario where pregnancy begins without protection—and the possibility of exposure arises.
How the Rubella (MMR) Vaccine Works for Women Pre-Pregnancy
The key tool is the MMR vaccine (measles-mumps-rubella), which includes rubella-containing component. According to the CDC: two doses of the MMR vaccine are recommended for optimal protection.
Here are the important features and guidelines for women of childbearing age:
-
Before conceiving, women should confirm rubella immunity (via documented vaccination or blood test).
-
If immunity is not confirmed, vaccination should occur before pregnancy. As a precaution, pregnancy should be avoided for at least 28 days (4 weeks) afterreceiving MMR.
-
Note: MMR vaccine is contraindicated during pregnancy because it’s a live-attenuated vaccine. Women who inadvertently receive the vaccine during pregnancy should discuss with their prenatal provider, but the evidence doesn’t currently support pregnancy termination.
Key Facts Every Woman Planning Pregnancy Should Know
-
Rubella infection in early pregnancy frequently leads to miscarriage, stillbirth or serious birth defects.
-
Vaccination coverage under ~80% can paradoxically increase risk of CRS by shifting infection to older ages (including pregnant women).
-
In some adult women (especially if not vaccinated or from regions where the vaccine wasn’t standard), susceptibility to rubella remains.
-
Women who are seronegative (no evidence of immunity) should receive the vaccine before pregnancy. If vaccinated postpartum, that’s also acceptable.
Addressing Common Concerns and Misconceptions
“Is it safe to get vaccinated if I might become pregnant soon?”
Yes — if you are not pregnant and you wait the recommended 28 days before conceiving. The vaccine is safe for non-pregnant women and offers durable protection.
“What if I discover I’m pregnant and I’m not immune to rubella?”
In this case, the vaccine cannot be given until after delivery. But your healthcare team can monitor you closely, counsel you on exposure risks, and plan postpartum vaccination.
“Does the vaccine cause birth defects if given during pregnancy?”
No clear evidence supports that. Studies of inadvertent vaccination during pregnancy have not shown increased birth defects. However, due to theoretical risk, vaccination during pregnancy is still avoided.
“I was vaccinated as a child—do I still need to worry?”
If you have documented two doses of MMR or proven immunity, no extra doses may be needed. But if your record is unclear, a simple immunity check or clinic discussion is advisable.
Implementation: What Women of Childbearing Age Should Do
Step 1: Review Your Vaccination History
Check if you received the MMR vaccine (or rubella-containing vaccine) and whether you have two documented doses or a blood test confirming immunity. If you were born in a region or time frame where rubella vaccination was not consistent, this is especially important.
Step 2: Ask Your Provider for Serologic Testing if Needed
Your provider may offer a rubella IgG antibody test to confirm immunity. If the result shows no immunity, vaccination is recommended before you plan pregnancy.
Step 3: Get Vaccinated at the Appropriate Time
If you’re non-pregnant, make an appointment for MMR vaccination. After vaccination, wait at least four weeks (28 days) before attempting pregnancy. This ensures your immune system has mounted full protection.
Step 4: Use Effective Contraception Until Immunity is Ensured
Following vaccination, continue contraception for the recommended safe interval. Then, once immunity is confirmed and you’re ready, you may proceed with pregnancy planning.
Step 5: Postpartum Women Should Be Checked
If you were not immune and then become pregnant—or if you were found susceptible during pregnancy—you should receive vaccination immediately after delivery (ideally before hospital discharge) to protect future pregnancies.
Broader Public Health Implications
When women of childbearing age remain non-immune, the community is at risk of a resurgence of rubella—and thereby CRS. The World Health Organization notes that in countries where vaccine coverage drops below 80%, infection may shift to older ages, increasing the risk for pregnant women.
By ensuring high immunization rates among reproductive-aged women, we not only protect individual pregnancies—but contribute to population-wide prevention of CRS outbreaks, safeguard vulnerable infants, and help maintain rubella elimination status.
Conclusion: A Critical Step for Maternal and Fetal Health
For women of reproductive age, the rubella vaccine is not merely optional—it is essential. By taking steps to confirm immunity, vaccinate when needed, and plan pregnancy accordingly, women protect themselves, their future children, and public health.
At Local MD, we emphasise that preconception care includes vaccination review as a key component. Our practice encourages all women planning pregnancy to talk with their healthcare provider about rubella immunity, ensure their records are up to date, and make vaccination part of their journey toward a safe and healthy pregnancy.
The rubella vaccine may seem routine—but for women who hope to conceive, it is one of the most impactful preventive measures available. Don’t leave your immunity to chance. Confirm it, secure it, and embark on your parenthood journey with confidence.